
New report: Progress in reducing malaria burden has stalled

Progress in reducing the burden of malaria remains stalled since 2015 after previous strong gains, reveals the latest data released overnight as part of the World Health Organization’s (WHO) World malaria report 2022.
There were an estimated 619,000 malaria deaths in 2021 (the 2022 report covers the previous calendar year) compared to an estimated 625,000 deaths in 2020.
The number of deaths in 2021 is still well up on the 568,000 deaths estimated for 2019, before the start of the COVID-19 pandemic.
There were an estimated total of 247 million malaria cases worldwide in 2021.
After almost a decade of significant gains, in the last few years progress has stalled, exacerbated further by the COVID-19 pandemic.
This latest data reiterates that there has been no progress in reducing the burden of malaria over the past five years, said Professor James Beeson, Burnet Deputy Director and Head of the Malaria Immunity and Vaccines Group.
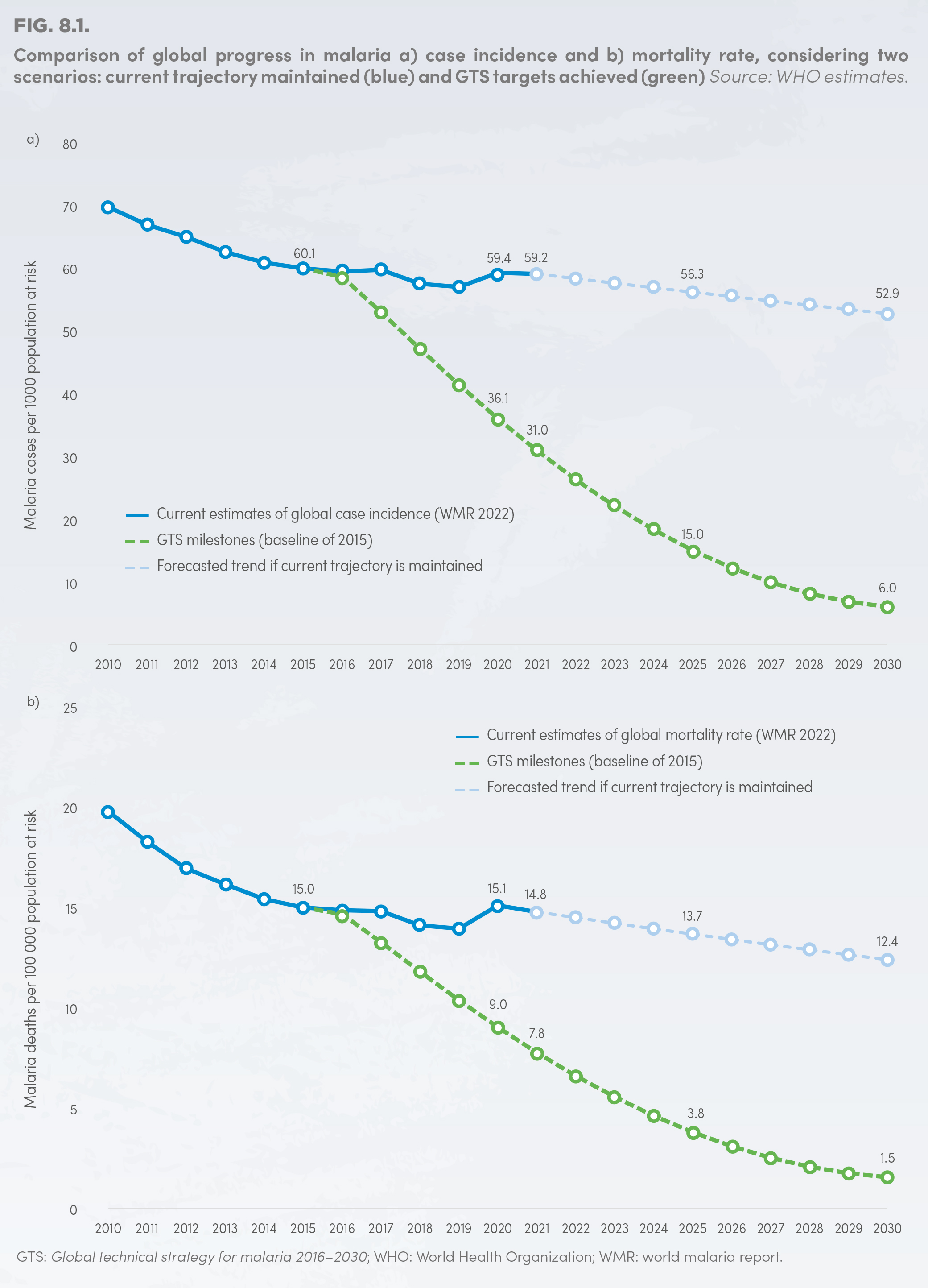
In 2015 the WHO set the ambitious goals of reducing both global malaria mortality rates and case incidence by at least 90 per cent by 2030, compared to 2015 levels.
But we’re not showing signs of progressing in that direction currently, Professor Beeson said.
At a regional level, Africa still shoulders the biggest malaria disease burden, accounting for 95 per cent of all cases and 96 per cent of all deaths in 2021 – nearly 80 per cent of which are children under five years old.
Southeast Asia had two per cent of the world’s malaria cases in 2021. The number of cases in Southeast Asia increased by 400,000 in 2021, and half of that increase was in Myanmar.
It was also the only WHO region to reach the 2020 milestone of a 40 per cent reduction in malaria case incidence and mortality, compared to the 2015 baseline.
In the Western Pacific region, 87 per cent of cases were in Papua New Guinea. But a 15 per cent rise in malaria cases that occurred during the first year of the COVID-19 pandemic was reversed with cases falling by 14 per cent between 2020 and 2021.
Professor Beeson said there are multiple reasons for why our progress against malaria has stalled.
“One is that we don’t have the tools or interventions that we need to really combat malaria and push it down, and ultimately eliminate it,” he said.
“And the second is that there’s not sufficient funding for malaria interventions – analysis shows the level of investment in malaria control and elimination efforts is about 50 per cent below what it needs to be.”
There’s a big funding gap in getting the current tools we have for combatting malaria to people and to develop better tools, said Professor Brendan Crabb AC, Burnet Director and CEO and Co-Head of the Malaria Virulence and Drug Discovery Group.
For example, we need better insecticides in bed nets as the malaria parasites are being resistant to the current insecticides used. And we need better diagnostics for malaria because the parasites are also learning to outsmart those.
“We need existing tools to be delivered better, and redouble our efforts around next-generation tools to do it easier,” Professor Crabb said.
While the Australian government has contributed over $970 million to the Global Fund to Fight AIDS, Tuberculosis and Malaria we need to up the ante, he said.
“Investment in reducing the malaria burden is an investment in health, wealth and security. It’s going to cost all of us more if the burden of malaria keeps going up,” Professor Crabb said.
“The reason for this is malaria is synonymous with poverty. Communities, regions and countries can’t escape that cycle with high burdens of malaria present, making those communities, regions and countries unstable and less productive than they otherwise would be.”
And then there’s the ongoing impacts of the COVID-19 pandemic which has severely impacted access to malaria services and procurement, said Professor Freya Fowkes, Burnet Deputy Program Director for Maternal, Child and Adolescent Health and Head of the Malaria and Infectious Diseases Epidemiology Group.
“It has also impacted the implementation of effective interventions, particularly in hard-to-reach geographically isolated populations which often harbour the greatest malaria burden,” she said.
Looking at the countries in our region, Professor Beeson said there are both positives and negatives to take from the report.
“In PNG, they’re facing a similar challenge to many countries in sub-Saharan Africa – a difficulty pushing malaria down and progressing towards elimination,” he said.
“Myanmar has made a lot of gains in malaria control in the last decade or so, but now faces a major challenge to regain control and get malaria elimination back on track.”
Cambodia, Vietnam and Thailand have also made major gains against malaria, thanks to sustained investment over many years, Professor Beeson said.
To arrest malaria transmission, we need new tools, new and better diagnostics, more protective, effective and longer-lasting vaccines, and better treatments and prevention methods, he said.
“These innovations alongside greater action on tackling malaria will give us a better chance of accelerating reductions in cases and mortality rates.”
Burnet is addressing this challenge through a recently funded collaborative project to develop multiple strategies to interrupt malaria transmission.
CLICK HERE to read the WHO’s World malaria report 2022.



